Needle biopsy is a crucial procedure in the diagnosis and treatment of pulmonary diseases. However, respiratory movement significantly affects the precision of traditional needle biopsy for lungs— “a millimeter off can mean a world of difference.” The procedure demands exceptional skill and experience from physicians.
How can the number of needle adjustments be minimized? How can complications be avoided to the greatest extent possible while reducing patient discomfort? Recently, Professor ZHOU Caicun’s team at Shanghai East Hospital, affiliated with Tongji University, has provided an answer.

Two years ago, Ms. WU underwent surgery at another hospital for poorly differentiated adenocarcinoma in the lower lobe of her left lung. Recently, her condition began to relapse. To develop an appropriate treatment plan, she needed a percutaneous tissue biopsy. However, the potential complications of the procedure caused her great concern.
“We have a new technology!” After a comprehensive assessment of the patient’s condition and concerns, Prof. ZHOU introduced her to the team’s latest innovation, the Lung Biopsy Surgery Navigation Robot, which is now being clinically applied.
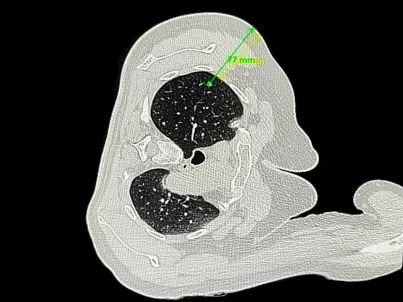
As the robot scanned her lung, imaging data was instantly transmitted to the navigation system, which reconstructed both two-dimensional images and a three-dimensional model of the lung. A coaxial needle precisely reached the planned target, allowing the physician to perform a biopsy on the lung lesion without causing any related complications.

This newly developed navigation robot integrates CT imaging with intelligent sensing technology. With a single scan, the system aligns the patient’s coordinate system with the navigation system’s coordinate framework. Based on the pre-planned surgical path, it then enables precise guidance and positioning of the biopsy instrument.
According to Prof. ZHOU, the clinical application of this system has shown a significant improvement in biopsy efficiency and a reduced risk of pneumothorax and bleeding. The procedure eliminates the need for adhesive markers, manual puncture point mapping, and stepwise needle insertion, shortening the conventional 30-minute lung biopsy to just 8 to 10 minutes.
Moreover, the robot does not alter physicians’ used way for needle biopsy, nor does it require the installation or calibration of special optical or electromagnetic accessories. Trained doctors can quickly and accurately operate the system. Meanwhile, concerns over CT scan frequency and radiation exposure—a key worry for patients—have been substantially alleviated.
The robot can be applied in biopsy procedures, ablation therapy, and pulmonary nodule localization surgeries. It received Class III certification from the National Medical Products Administration (NMPA) in early 2024. Last August, the research team presented an oral report on this technology at the ASCO Breakthrough Summit, and their clinical trial results were recently published in the prestigious oncology journal Lung Cancer.
“Medical research and innovation must ultimately align with real clinical needs,” said Prof. ZHOU. “By conducting extensive and in-depth clinical studies and applications, we can better integrate new technologies into clinical practice to serve patients more effectively.”
